The Nuremberg Code
Medical Ethics
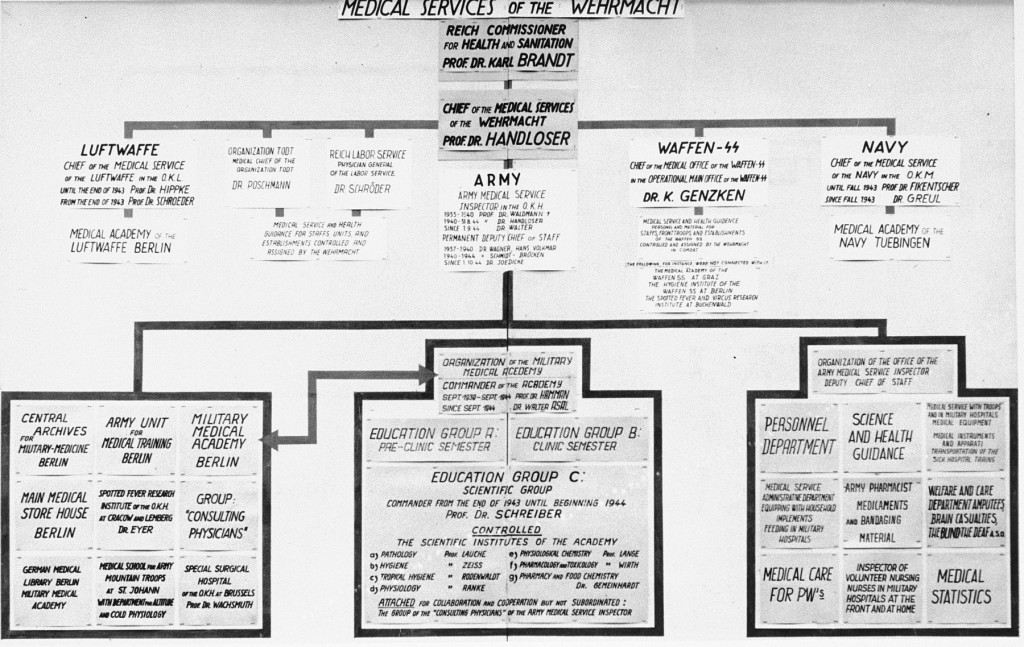
Medical professionals were put on trial after the war for their participation in war crimes and crimes against humanity during the Holocaust. The trial sparked questions about medical ethics in the aftermath of the brutal experiments on prisoners in the camp system.
On December 9, 1946, an American military tribunal opened criminal proceedings against 23 leading German physicians and administrators for their willing participation in war crimes and crimes against humanity. This case is known as the "Doctors Trial" (USA v. Karl Brandt et al.). On August 19, 1947, the judges of the tribunal delivered their verdict. But before announcing the guilt or innocence of each defendant, they confronted the difficult question of medical experimentation on human beings.
Several German doctors had argued in their own defense that their experiments differed little from those conducted before the war by German and American scientists. Furthermore they showed that no international law or informal statement differentiated between legal and illegal human experimentation. This argument was a great concern to two US doctors who had worked with the prosecution during the trial, Dr. Andrew Ivy and Dr. Leo Alexander.
As a result, on April 17, 1947, Dr. Alexander submitted a memorandum to the United States Counsel for War Crimes. The memo outlined six points that defined legitimate medical research. The trial's verdict of August 19 reiterated almost all of these points in a section entitled "Permissible Medical Experiments." It also revised the original six points into ten, and these ten points became known as the "Nuremberg Code."
In the half century following the trial, the code informed numerous international ethics statements. Its legal force, however, was not well established. Nevertheless, it remains a landmark document on medical ethics and one of the most lasting products of the "Doctors Trial."
Permissible Medical Experiments
From the trial transcript
The great weight of the evidence before us is to the effect that certain types of medical experiments on human beings, when kept within reasonably well-defined bounds, conform to the ethics of the medical profession generally. The protagonists of the practice of human experimentation justify their views on the basis that such experiments yield results for the good of society that are unprocurable by other methods or means of study. All agree, however, that certain basic principles must be observed in order to satisfy moral, ethical and legal concepts:
1. The voluntary consent of the human subject is absolutely essential.
This means that the person involved should have legal capacity to give consent; should be so situated as to be able to exercise free power of choice, without the intervention of any element of force, fraud, deceit, duress, over-reaching, or other ulterior form of constraint or coercion; and should have sufficient knowledge and comprehension of the elements of the subject matter involved as to enable him to make an understanding and enlightened decision. This latter element requires that before the acceptance of an affirmative decision by the experimental subject there should be made known to him the nature, duration, and purpose of the experiment; the method and means by which it is to be conducted; all inconveniences and hazards reasonably to be expected; and the effects upon his health or person which may possibly come from his participation in the experiment.
The duty and responsibility for ascertaining the quality of the consent rests upon each individual who initiates, directs or engages in the experiment. It is a personal duty and responsibility which may not be delegated to another with impunity.
2. The experiment should be such as to yield fruitful results for the good of society, unprocurable by other methods or means of study, and not random and unnecessary in nature.
3. The experiment should be so designed and based on the results of animal experimentation and a knowledge of the natural history of the disease or other problem under study that the anticipated results will justify the performance of the experiment.
4. The experiment should be so conducted as to avoid all unnecessary physical and mental suffering and injury.
5. No experiment should be conducted where there is an a priori reason to believe that death or disabling injury will occur; except, perhaps, in those experiments where the experimental physicians also serve as subjects.
6. The degree of risk to be taken should never exceed that determined by the humanitarian importance of the problem to be solved by the experiment.
7. Proper preparations should be made and adequate facilities provided to protect the experimental subject against even remote possibilities of injury, disability, or death.
8. The experiment should be conducted only by scientifically qualified persons. The highest degree of skill and care should be required through all stages of the experiment of those who conduct or engage in the experiment.
9. During the course of the experiment the human subject should be at liberty to bring the experiment to an end if he has reached the physical or mental state where continuation of the experiment seems to him to be impossible.
10. During the course of the experiment the scientist in charge must be prepared to terminate the experiment at any stage, if he has probable cause to believe, in the exercise of the good faith, superior skill and careful judgment required of him that a continuation of the experiment is likely to result in injury, disability, or death to the experimental subject.
Footnotes
-
Footnote reference1.
From: Trials of War Criminals before the Nuremberg Military Tribunals under Control Council Law No. 10. Nuremberg, October 1946–APRIL 1949. Washington, D.C.: U.S. G.P.O, 1949–1953.
Critical Thinking Questions
How did German professionals and civil leaders contribute to the persecution of Jews and other groups?
Besides medical professionals, what other professionals were charged with crimes in the wake of the Holocaust?
Beyond the verdicts, what impact can trials have?
Research whether other professional codes of conduct changed after the Holocaust.